In this post we discuss why your Achilles tendon injury is not getting better and what you can do now. Whilst originally written with runners in mind, it will serve anybody who’s suffering with Achilles tendon issues.

Before I show you how you can achieve results like this, let’s take a look at what’s likely going on in your Achilles tendon and why what you’ve tried already hasn’t worked.
Most contemporary research shows Achilles tendons that have been sore for some time (3 months plus) are in a state of degeneration. In other words the tendon is not in an inflammatory state (Achilles Tendinitis) but rather one of disorganisation (Achilles Tendinosis).
This sounds worrying but don’t panic, the process is entirely reversible with the right approach.
Tendons, like the muscles they attach to require force to stay healthy. The stimulus must be at just the right level however. Too little and too much both create issues.
If you’re reading this and you’re a runner then the chances are you’ve overloaded the muscles of your lower leg at some point. While it may have gone unnoticed at the time, it was this that set the scene for your present predicament.
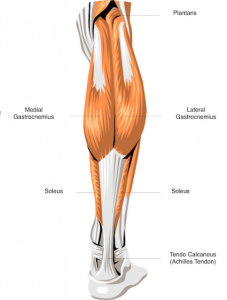
Since that point you’ve been running with muscles in your lower leg that are both unable to produce force or attenuate it appropriately. Both to the detriment of the structure that attaches them to your calcaneus, your Achilles tendon.
The value of every rehabilitation protocol must therefore be assessed with this in mind.
How will it improve the ability of your plantarflexors (calf muscles) to contract so you can begin to place controlled forces through your Achilles tendon again? It’s this that will effectively kick start the process of regeneration within the tendon.
With that in mind, let’s take a look at what you’ve probably tried so far.
Rest
Doing nothing has many benefits, you can get through a box set, hang out with your family a bit more, and get a few jobs done around the house.
It probably won’t magically cure your Achilles tendon however. Even if it reduces the pain for a while, the moment you begin to run again it will likely return because nothing has significantly changed.
Stretching
The fact that I even have to debunk stretching as a rehab method for Achilles tendon issues is irritating. There is no evidence that stretching works for the prevention or treatment of any injury let alone Achilles tendinopathies.
It still appears in every rehab article I read on the subject however. Not only is it ineffectual, it’s also potentially problematic.
Take a read of this from a recent Runners World article on the issue of Achilles tendon rehab. This, believe it or not, is from a podiatrist who was actually promoting the use of stretching.
‘Damage occurs when the tendon is stretched 4 percent beyond its strain level and rupture occurs at 8 percent beyond its relaxed state. For the normal tendon, that’s only about a quarter of an inch. Therefore it’s very important only to feel the stretch in the calf muscles.’
Good luck judging exactly where a quarter of an inch is when you’re hanging off the edge of a step. Ridiculous. Stretching will only make you weaker. Stop it.
Corticosteroids, NSAIDs or any drug for that matter
The use of taking any anti inflammatory drug, be it orally or via injection is instantly called into question when you know that there is unlikely to be a significant inflammatory process occurring if the issue has become chronic in nature.
Whilst drugs may provide an analgesic effect, their long term use merely allows you to damage the tendon further without knowing about it. This is rather like turning the red light off on the dashboard and continuing to drive your car.
Massage
Massage certainly feels nice to some people. Being touched while being listened to might be beneficial on some level but evidence that this will solve your Achilles tendon problems doesn’t exist unfortunately.
Whilst it may promote relaxation and improve your mood, don’t expect a miraculous return to running. I would be especially wary of any massage strong enough to cause pain, this can be counterproductive.
Eccentric strengthening
This is the exercise you will have been given if you’ve visited a physiotherapist for your Achilles tendon problem. It’s certainly more effective than anything else I’ve mentioned so far.
The exercise involves loading the eccentric phase (lowering the heel to the floor) of a calf raise which has been shown to promote healing of the Achilles tendon in some cases.
The weakness of this method is two fold; firstly the weakened muscles of the calf may not be able to tolerate this much force which will only exacerbate your Achilles tendon pain.
Secondly, a full return to running will also require the plantarflexors to shorten under load. A motion not trained with this approach.
Think of it as half right which will explain it’s 60% success rate in studies with injured runners.
Orthotics
Imagine you had a knee that was deemed to extend too far and you were told to put a brace on it in order to prevent that motion from occurring.
Not only would it cramp your style, it would also impede the ability of your leg to both absorb and produce force. It would also probably cause issues somewhere else in your body.
Sticking a post in your shoe to prevent motion at your foot is no different.
Work on your muscular system first before even thinking about this as an option. I see plenty of people that are still trying to recover from running around with their feet braced.
Ultra sound, extra corporeal shock wave therapy, electrolysis
All these therapies are designed to kick start the healing process in one way or another, although evidence for their effectiveness is thin on the ground.
Think back to the original problem and you can see why. How do they positively influence the ability of your plantarflexors to contract? Answer, they don’t.
A different approach to Achilles tendon issues
Whilst it’s very difficult to provide a rehab programme based on your individual strengths and weakness, some of which won’t just be at your ankle. It is possible to provide you with both the thought process and some of the exercises I use to improve Achilles tendon issues.
Before placing any amount of force through an injured area, it’s necessary to improve the ability of muscles likely affected by the injury to contract. In this case muscles that plantarflex the ankle as we have already discussed. This is best done with isometrics.
Isometrics are exercises that change neither the angle of the joint they act upon or the length of the target muscle.
They are an effective way of improving communication between the target muscle and the central nervous system.
It’s this communication that may have been affected by the injury and the reason why jumping straight into exercise doesn’t always work.
Isometrics for Achilles tendon issues
Plantar flexion isometric
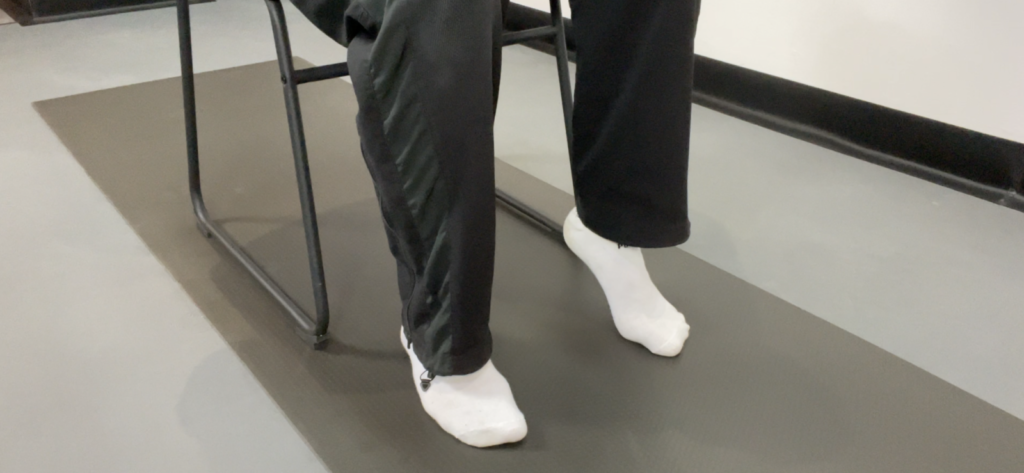
Take a seat in a chair and slowly lift the heel of the affected side away from the floor. When you reach the top position hold for 6 seconds focusing on your calf muscles.
Lower back to the floor and repeat a further 5 times, each time trying to lift your heel a little further from the floor without lifting the knuckle of your big toe.
Dorsiflexion isometric

Now try lifting the front of your foot away from the floor. Again hold for 6 seconds and if you’re able curl your toes down to make the exercise more challenging. Repeat a further 5 times each time trying to lift your foot closer to your shin.
Strengthening exercises for Achilles tendon issues
Seated calf raises

Performing calf raises from this position is usually more tolerable if your Achilles tendon is particularly sore.
Start without additional resistance to begin with and add dumbbells or a straight bar on the top of your thighs providing the movement is pain free. Use a weight that will bring about mild fatigue in your calf muscles but which doesn’t irritate your Achilles tendon.
Aim for 2 sets super slow 5 sec up and 5 sec down for 6-8 repetitions.
Standing calf raises
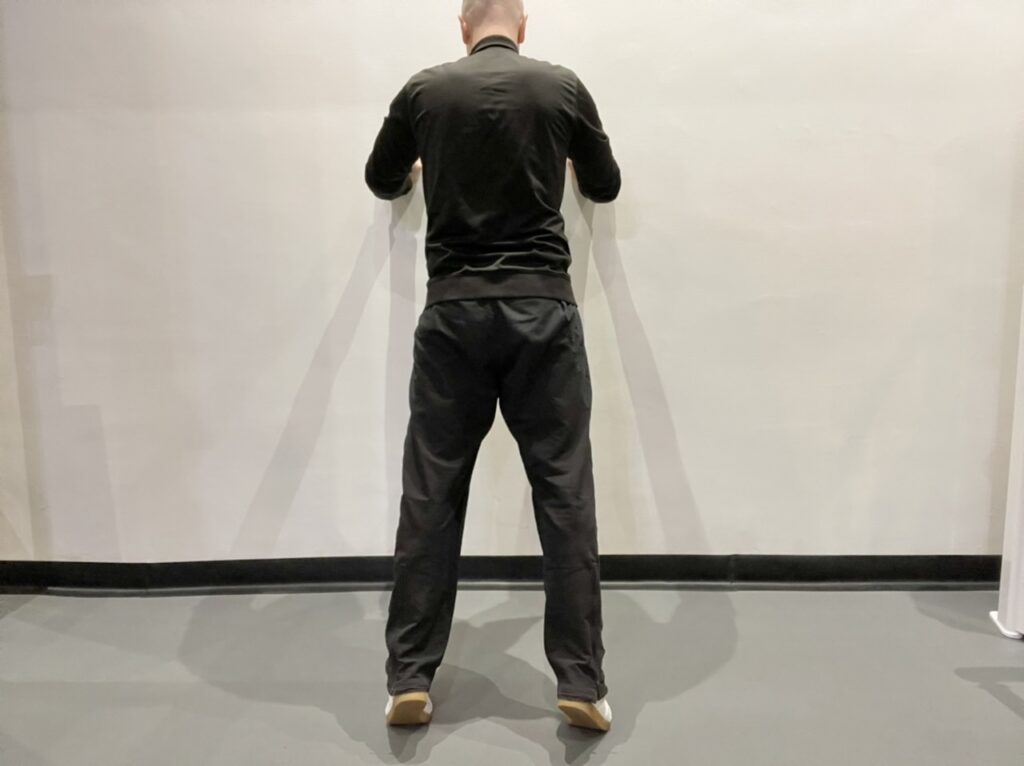
Once you’ve built some strength in your calf muscles move to the standing version.
Stand with feet shoulder width apart close to a wall for stability. Slowly rise up onto the balls of your feet before slowly returning to just above the floor and repeating.
Again use the same 5 seconds up and 5 seconds down timing and aim to complete 2 sets of 6-8 repetitions.
Standing single side eccentric heel drops
The next progression is to try lowering yourself with just one leg.
Make sure you still use both legs to return to the top of the movement however. Use a slightly quicker concentric phase of 3 seconds and an eccentric phase of 5 seconds again on the single leg.
Aim for 2 sets of 8-10 repetitions.
Summary
Chronic Achilles tendon pain in runners is likely a result of overload to the soleus and gastrocnemius muscles.
Any effective rehabilitation programme must first restore the ability of these plantarflexors to contract appropriately, before aiming to strengthen them.
This will begin to provide your Achilles tendon with the stimulus it requires to regenerate.